
THEN & NOW
1970, 2018
Burns are among the nastiest wounds a person can experience, and the Army’s Burn Center has been working for more than 70 years to develop treatments that speed healing and recovery.
by Ms. Jacqueline M. Hames
A Soldier sustains devastating third-degree burns over 70 percent of her body when her Humvee is hit with an improvised explosive device. Her excruciating injuries leave her at risk for infection, terrible scarring and death. After being stabilized in the field, she is medically evacuated to the Army’s closest burn center, where highly trained surgeons treat her wounds, ensuring that she is protected from infection and organ failure. There, they can even give her brand-new skin to replace what was lost.
This is the future of Army burn treatment at the U.S. Army Institute of Surgical Research Burn Center at Joint Base San Antonio – Fort Sam Houston, Texas.
Renowned worldwide in 1970 for its cutting-edge treatment of thermal injuries—burns—the Burn Center proved the efficacy of a new burn cream, pioneered wound treatment and perfected skin grafts by that year, its 25th anniversary. Now entering its 73rd year, the Burn Center has not only maintained its reputation but continues to innovate with new skin substitutes and replacements, resuscitation techniques and inhalation injury mitigation.
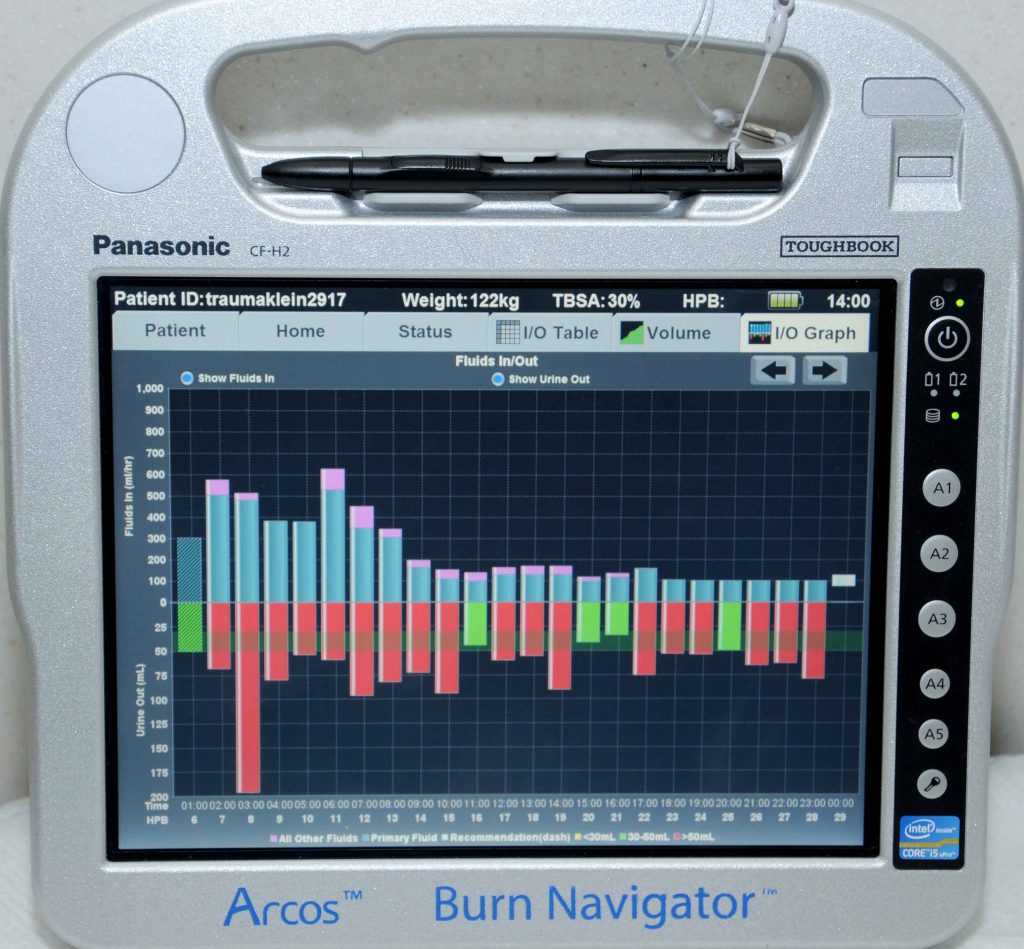
To avoid giving burn patients too much intravenous fluid, which can create swelling that can cause life- or limb-threatening complications, the Burn Center developed Burn Navigator, manufactured by Arcos Medical Inc. The bedside computer helps guide resuscitation in burn patients. (U.S. Army photo)
BURN BUTTER
The antimicrobial burn cream Sulfamylon was introduced in January 1964, said Dr. Leopoldo C. Cancio, director of the Burn Center. The sulfonamide drug family, of which Sulfamylon is a member, is used to treat bacterial infections like bronchitis, eye infections and bacterial meningitis. That family of drugs has been around for decades, and the active ingredient in Sulfamylon, mafenide acetate, was not new. But using it as a cream to prevent infections in burn wounds was.
“Surgical Research Institute Enters 25th Year of Burns Research,” a February 1970 article in Army Research and Development Newsmagazine, the predecessor to this magazine, detailed how, after extensive laboratory study, investigators at the Burn Center put the drug into a water-soluble white cream to be applied topically to burned areas.
“That is the compound which that article refers to as ‘burn butter,’ and it is used to this day for the treatment of burn wounds,” Cancio said. “Since then, there have been a lot of other products that have come out and that we use for burn wounds treatment, but Sulfamylon was really the first and foremost of those treatments.”
In the 1940s and ’50s, an otherwise healthy adult with burns over 40 percent of his body had a 50-50 chance of surviving, said Dr. Basil A. Pruitt, former commander and director of the Burn Center. The survival rate improved by 1970; that year Pruitt, then a lieutenant colonel, told reporters that Sulfamylon successfully prevented infection in second- and third-degree burns covering up to 60 percent of the body, and reduced the bacteria count in burn wounds more effectively than any other known topical application.
“Today, if you have an 80 percent burn, you have a 50-50 chance of living or dying, and that’s real progress,” Pruitt continued. “That’s statistically documentable progress.” The medical staff at the Burn Center is responsible for that progress.
TREATMENT AND CARE
The delayed approach to surgery at the Burn Center in the 1970s meant leaving a burn wound open and debriding it—removing dead, damaged or infected tissue—daily in hydrotherapy to prepare the patient for a graft. While that approach was sound, it still left patients open to the risk of infection, even when Sulfamylon was applied.
“We don’t do that anymore,” Cancio said. Now, the center performs excision—the surgical removal of dead tissue—as soon as possible, especially if the patient has deep wounds, before grafting with the patient’s own skin or a homograft—donor skin.
Speed of care is a key factor with burn wounds, Pruitt said. If burned and dead tissue remains on the patient, it not only can increase the risk of infection, but also increase the amount of scarring that could occur, particularly if the wounds are deep. “You take it off, it limits any extension of tissue destruction by any invasive bacteria,” he said.
Another key factor in burn care is the patient’s ability to heal. Accelerating wound healing, particularly in patients with extensive wounds, is a goal of the Burn Center. Two future technologies, ReCell and StrataGraft, are closest to accelerating healing, Cancio said.
“ReCell is a technology in which we take a small biopsy of the patient’s normal skin, we scrape off the epidermal cells from that biopsy, we dilute them in a solution and we spray it onto the freshly excised wound bed. And those little skin cells grow and populate the wound bed and replace it with skin. So, sometimes ReCell is referred to as spray-on skin,” he said.
ReCell has completed Phase III clinical trials, meaning that the Burn Center is waiting to hear from the U.S. Food and Drug Administration and the manufacturing company that the product is available for purchase and, therefore, clinical use. “As I understand, that will happen pretty soon,” Cancio said.
StrataGraft is a ready-made, off-the-shelf skin substitute comprising two layers. One layer is an epidermal component—the outermost layer—and the other layer is a dermal component, the layer of tough connective tissue beneath the surface. “The epidermal component is derived from an immunologically privileged epidermis from neonates called NIKS cells. Those cells will not be immunologically rejected by the patient, unlike every other type of skin we might transplant from somebody else to a patient,” Cancio said.
NIKS, or near-diploid immortalized keratinocyte skin, is made with keratinocytes, cells that make up the vast majority of natural human skin and primarily protect skin from environmental damage, like bacteria.
NIKS cells used in the StrataGraft treatment “are basically a special type of skin cell that comes from somebody else and we put them on the patient’s excised wound bed and, ideally, this technology will go ahead and become part of the patient. And then over time, the patient’s own skin cells will grow into the product and replace the epidermal cells from somebody else with the patient’s own cells,” Cancio said.
StrataGraft is still in clinical trials, Cancio said. The Burn Center is participating in two of those trials; one to evaluate the product in patients with partial-thickness (second-degree) burns and another to evaluate the product in patients with full-thickness (third-degree) burns.

The Burn Center participated in the clinical trials of ReCell, a technology that deconstructs a small biopsy of a patient’s skin and dilutes it in a solution that can then be sprayed onto a wound. From there, the patient’s skin cells will populate the wound and regrow skin. (U.S. Army photo)
UNIVERSAL MODEL
The Burn Center has expanded its mission in the decades since 1970, from focusing almost exclusively on burns to encompassing many aspects of mechanical trauma as well as burn injuries.
“In a very real sense, the burn patient is the universal trauma model,” Pruitt said. “That is, everything that happens in the burn patient, in terms of organ system dysfunction, pretty much happens in mechanical trauma patients.” Patients who are shot, for example, experience the same changes that burn patients experience, except that mechanical trauma patients’ experiences are accelerated, causing life-threatening changes at a faster rate.
“So, the mission of the unit has expanded to include all of trauma, including combat injury patients, and it has, in the last several years, become the center of combat casualty care research by the integration of all three military services, Army, Navy and Air Force,” he said.
The National Defense Authorization Act for Fiscal Year 2017 mandated that the primary mission of the military health system is readiness, Cancio said. The center continuously brings in medical personnel from all over the armed services for team training. “We believe that this burn center contributes significantly to training people to be prepared to deploy to the combat zone and take care of severely injured patients,” he said.
The complexity of burn care is not just restricted to a skin problem. Major burns impact all organs and systems of the body, Cancio said, from the psychological, to the heart, lungs, kidneys and the patient’s ability to function from a physical and occupational therapy standpoint. “All those organ systems are affected by burn injury, so whether you’re a critical care nurse, a surgeon, whether you’re an occupational physical therapist or another therapist, respiratory therapist, you get excellent exposure to very critically ill patients at this Burn Center, so we feel that our training mission has only intensified with the publication of a mandate to focus on readiness,” Cancio said.
In recent years, the Burn Center hosted eight Japanese doctors who have gone on to be prominent burn surgeons and trauma surgeons in their home country, Pruitt said. Two Belgian army surgeons came to study, staying for six months each. The center also hosted the surgeon general of Norway, he said.
CONCLUSION
Pruitt, who retired from the Burn Center as a colonel after 27 years there, still teaches surgery at the Burn Center one day a week. He is particularly interested in the research and clinical studies the center has expanded into, such as the proper amount of resuscitation (intravenous) fluid for patients, computer-guided resuscitation and the mitigation of inhalation injury. Cancio is active in the management of the inhalation injury and computer-guided resuscitation programs.
During the early parts of the wars in Iraq and Afghanistan, medical staff at the Burn Center noticed some burn patients were receiving too much resuscitation fluid in the first 24 to 48 hours after injury, Cancio said. The fluid is required to replace ongoing losses to the injured tissue and elsewhere in the body. “Some patients received a quarter of their body weight in saltwater over one day. When this fluid leaks into the arms, legs or abdomen, too much swelling can cause life- or limb-threatening problems,” he said.
To help avoid over-resuscitation and better guide resuscitation decisions, the Burn Center developed a computer called Burn Navigator, manufactured by Arcos Medical Inc. of Houston. “This product made it through the Army product acquisition process for use in battlefield medical treatment facilities and is also available commercially around the world,” Cancio said.
Combat casualties in the same wars experienced smoke inhalation injury rates that were twice as high as those in civilian burn centers because of the use of improvised explosive devices on personnel in vehicles. “To improve the care of patients with these and other severe lung injuries, the Army Burn Center became the home of a new program in adult extracorporeal membrane oxygenation [ECMO],” he said. ECMO uses a pump to circulate blood through an artificial lung, removing carbon dioxide and oxygenating blood cells, which reduces the stress on the patients’ organs and helps them heal.
Cancio is quick to say that much has happened in the years since the publishing of the 1970 article and that there are many good burn centers across the country and worldwide; however, “many of the directors of burn centers across the U.S. in fact trained at this burn center throughout the period of time both before and after the article was written, and I think that’s one of the big contributions of this burn center to the quality of burn care. It didn’t just stay at one center, but it extended to other places through the training efforts of our predecessors,” he said.
Pruitt believes the Burn Center has had a demonstrable effect on the survival of many burn patients who otherwise would have died without the advances in clinical care and research the Burn Center provided over the years. In conventional warfare, particularly if there are lots of armored fighting vehicles, the number of burns ranges from one in 20 to one in five casualties, Pruitt said. “That’s why the Army has a real reason to continue to be the leader in burn and trauma research … the high incidence of burn injury as related to the type of warfare involved is a real reason for maintaining the support of the Institute of Surgical Research and Burn Center.”
For more information, go to http://www.usaisr.amedd.army.mil/12_burncenter.html.
JACQUELINE M. HAMES is a writer and editor with Army AL&T magazine. She holds a B.A. in creative writing from Christopher Newport University. She has more than 10 years of experience writing and editing for the military, with seven of those years spent producing news and feature articles for publication.
Related Links
AVITA Medical Announces Presentation of RECELL Device Clinical Trial Results, BusinessWire, June 26, 2018: https://www.businesswire.com/news/home/20180626006659/en/AVITA-Medical-Announces-Presentation-RECELL%C2%AE-Device-Clinical
StrataGraft Skin Tissue in the Promotion of Autologous Skin Regeneration of Complex Skin Defects Due to Thermal Burns That Contain Intact Dermal Elements, U.S. National Library of Medicine: https://clinicaltrials.gov/ct2/show/NCT03005106?term=stratagraft&rank=3
American Burn Association: http://ameriburn.org/who-we-are/governance/
This article will be published in the October – December 2018 issue of Army AL&T magazine.
Subscribe to Army AL&T News – the premier online news source for the Army Acquisition Workforce.
![]() Subscribe
Subscribe

