
In future conflicts, with communication channels and evacuation routes contested, a lot more casualty care might happen right there on the battlefield itself.
by Mr. Ramin A. Khalili
Dr. Elliot Botvinick sits in his office on the campus of the University of California, Irvine, holding a tiny device in the palm of his hand. It is smaller than a garage door opener, smaller than a standard business card even, and is so slight and inconspicuous that he might be able to stick one on a passing student without their noticing.
It also might be the future of battlefield medicine, according to the U.S. Army.
Minds like Botvinick’s may be exactly what’s needed to conquer approaching combat scenarios that experts predict will look starkly different than the current version, ones where the efficient use of targeted medical knowledge may be the single most important key to victory.
Botvinick’s handheld lactate monitor fits in perfectly then, as it features a wearable, subcutaneous microsensor designed to detect lactic acid levels, which rise in the body during episodes of critical illness and internal bleeding, both of which exhibit symptoms that aren’t always visible to the naked eye.
“We’re feeling pretty confident,” said Botvinick, a biomedical engineer. But while he is modestly optimistic, the Army expresses its faith in new medical technologies with a bullhorn.
To hasten the monitors’ delivery, the Army is looking to the Combat Casualty Care Research Program (CCCRP) of the U.S. Army Medical Research and Materiel Command (USAMRMC). “Our focus is squarely and specifically on the health and welfare of the warfighter,” said Col. Michael Davis, the newly installed CCCRP director.
In his role as an investigator with the CCCRP’s portfolio for Photonics and Light-Based Innovation for Severe Injury, Botvinick’s lactate monitor satisfies the Army’s desire for smaller, better technologies to operate in combat scenarios that will likely play out in denser, more urban areas, and in which prolonged field medical care will likely be the norm.
“The vision [for the device] is something like a blister pack that you would peel open in the field and then a medic would just slap it on the body,” says Botvinick. “And in that simple act of slapping, an insertion needle would be guided just under the skin […] and then by pulling back on a sticker or tab, that needle would be removed and just a flexible fiber would remain.”
That tiny fiber would then interrogate the tissue around it, asking how much lactic acid exists in the area, according to Botvinick. From there, the assembled information would then be transmitted via Bluetooth technology to a wearable unit on the skin.
While measuring lactate is not currently the standard of care in the field (chiefly because current protocol requires blood samples to be drawn and then sent to a lab for study, a logistical nightmare in the field), Botvinick’s sensor measures lactate faster than the lactate level within the body can change, which makes it ideal for the fluidity of long-term transport situations, as well as transportation between levels of care. As such, a number of prototype devices are being prepared for shipment to the U.S. Army Institute of Surgical Research in San Antonio for animal model testing.
This is just one example from a research program rich with potential solutions.
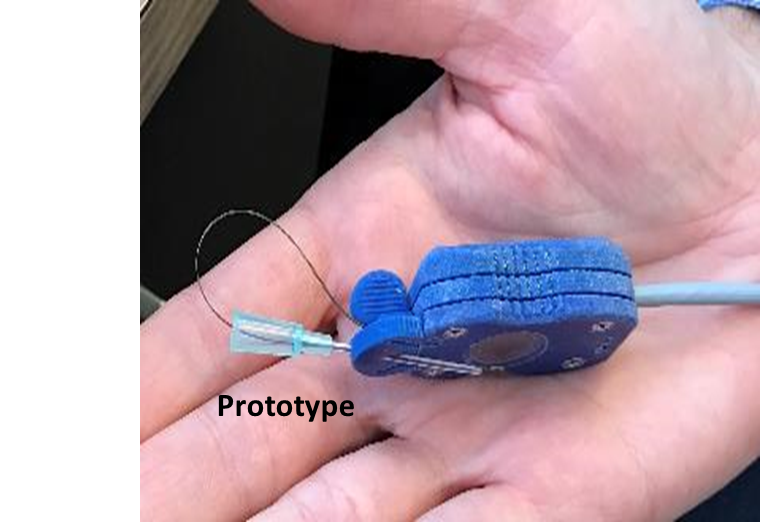
The U.S. Army believes the continuous lactate monitor, a prototype of which is shown here and features a wearable, subcutaneous microsensor designed to detect lactic acid levels, might be the future of battlefield medicine. (Photo by University of California, Irvine)
BATTLEFIELD MEDICINE
Based in a small building on the southern edge of Fort Detrick, Maryland, the CCCRP is the only federal entity specifically tasked with developing the tools and knowledge required to aid injured warfighters on the battlefield. It comprises four portfolio management areas: Hemorrhage and Resuscitation; Neurotrauma and Traumatic Brain Injury (TBI); Joint Forward Surgical-En Route Care; and the aforementioned photonics portfolio.
The Army is leaning on CCCRP to produce the next-generation tools it will need to conquer and secure the rather bleak battlefield projected for the 2025-2040 timeframe. Specifically, experts predict the U.S. will likely encounter far more sophisticated enemies in the future than in previous conflicts, as well as enemy forces with the capabilities to degrade and inhibit U.S. air, maritime, cyberspace and EMS access and superiority.
That puts the execution of prolonged field care in the spotlight. A recent Capability Needs Assessment commissioned by military leadership named prolonged field care as the No. 1 capability gap across the entire Army. Indeed, experts say future battlefields will require medical efforts to be more assertive at the point of injury as opposed to standard forward aid locations, a shift that also radically changes the concept of the “golden hour” standard of care, which relies on traditional medical transport to get service members treated within the first hour after injury.
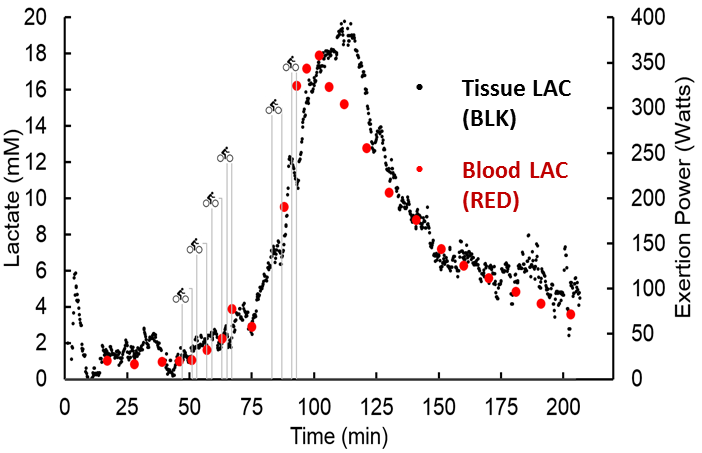
A readout of lactate measurement levels over time as provided by a continuous lactate monitor. Lactic acid levels rise during episodes of critical illness and internal bleeding, which may not be visible to the naked eye. (Photo by University of California, Irvine)
LITERALLY, ON THE BATTLEFIELD
“We’re going to need lighter, leaner, better capabilities than we currently have,” said Col. Antoinette Shinn, manager of the CCCRP’s joint Forward Surgical-En Route Care portfolio. “For instance, how are we going to maximize tele-health efforts in ways that will assist a far-forward medic, or maybe even no medic at all, in providing life-sustaining care for up to 72 hours?”
Shinn’s portfolio is currently investing heavily in noninvasive hemorrhage detection capabilities for situations in which a warfighter sustains an injury but is neither overtly bleeding nor visibly symptomatic yet. The latter falls into the burgeoning area of “intelligent tasking,” whereby physiology will ultimately determine a patient’s medical needs.
A more fully realized version of the CCCRP’s technological vision for the future is in the program’s Neurotrauma and Traumatic Brain Injury portfolio, where a slew of recent investments have evolved into a variety of potential solutions, each with substantial benefits. With more than 370,000 cases of TBI across all military branches since 2000, progress in this discipline is a top priority.
“We’ve got a number of promising technologies, but it’s not going to be just one of them that has all the answers for all environments,” said portfolio manager Dr. Tammy Crowder. “It’s not going to be like the chickenpox vaccine where everybody gets the shot and then we’re all protected.”
The portfolio’s standout performer so far has been the I-Portal PAS tool, developed by Pennsylvania-based Neuro Kinetics Inc. (NKI). The device uses a virtual-reality headset to assess possible brain injury by measuring a series of oculo-motor pathways, or, more simply, basic eye movement. The user completes more than two dozen tests over 25 minutes, after which a clinician analyzes eye movement and effective neuro-functional capability to determine if a TBI is present. Following initial feedback, NKI is in the process of reducing the exam time from 25 minutes to five while using the same battery of tests.
Crowder’s team is looking for other technologies as well, including balance boards and additional virtual-reality devices that measure separate oculo-motor pathways.
“We’re literally throwing the long ball with this one,” said Crowder. “But these kinds of efforts will hopefully enable first responders to offer more complete care.”
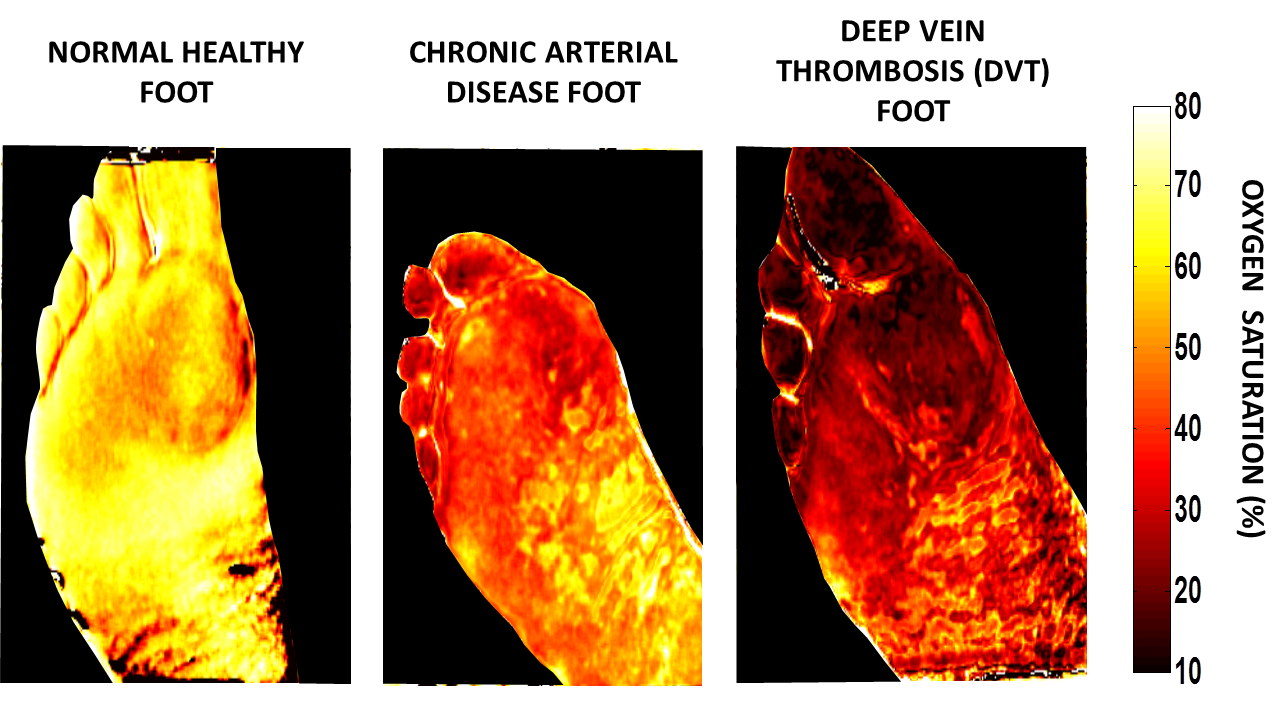
The images of an affected burn area produced by an SFDI surgical camera show parameters such as oxygen saturation, water content and total hemoglobin. (Photo by University of California, Irvine)
‘MOTHER NATURE GETS CONFUSED’
For Dr. Lynn Drake, a faculty member at Harvard Medical School and the Wellman Center for Photomedicine at Massachusetts General Hospital, both in Boston, partnering with the U.S. military requires a commitment to accuracy and consistency and a forward-leaning mindset.
“We’ve got about 23 clinical inventions that are now in use worldwide,” said Drake, an investigator with the CCCRP’s photonics portfolio, “plus another 14 platform technologies that have multiple applications, and then I’ve got another 60 things in our pipeline.”
One of those technologies is a cutting-edge fractional laser developed specifically with the military community in mind. In essence, the laser helps to remodel painful scars by creating thousands of tiny holes on the scarred area, which data shows heal faster and cleaner than the original wound.
“Mother Nature gets confused when she tries to heal a bigger wound,” Drake said, adding that fractional lasers are used in the medical community to reduce pain, minimize disfigurement and even erase some scars entirely. That same technology might be used for future skin-grafting efforts and other therapies. Devices for this kind of skin grafting have U.S. Food and Drug Administration (FDA) approval and are commercially available.
The Wellman Center has been partnering with DOD for 20 years, and currently more than 20 percent of its overall efforts are dedicated to the well-being of the warfighter.
The lab is also working to use light to make blood platelets last longer. “The military came in one day and said, ‘We need a way of making platelets last longer,’” said Dr. Conor Evans, a faculty member at Wellman. “And so now we have a project underway that we think will extend platelet storage time dramatically.”
That research is all the more important given the forecast for future battlefield scenarios where evacuation to external care facilities may not be immediately possible. According to the CCCRP’s Hemorrhage Control and Resuscitation portfolio, current investments are geared toward developing an FDA-approved dried plasma product, while the goal for future blood products is to ensure survivability for at least 6 to 12 hours—a number that jumps to 72 hours for potential prolonged field care scenarios. According to Evans, the early data is “fairly outstanding.”

A clinician operates an SFDI unit, which is being developed and commercialized by California-based Modulated Imaging Inc. and uses the principles of diffuse optical spectroscopy to determine whether burned tissue is suitable for reconstructive surgery. (Photo by University of California, Irvine)
WHEN PHYSICAL, PSYCHOLOGICAL MEET
Back at UC Irvine, the conversation grows subdued as it turns to treating burn injuries. While injuries thought to be fatal just a few years ago are no longer considered as such, burns are still complicated by infection and other variables. For Dr. Anthony Durkin, associate professor at the university and the adjoining Beckman Laser Institute and Medical Clinic, relief for burn victims is as much a matter of tissue as it is time.
“Burns are psychologically difficult,” said Durkin, an investigator with the CCCRP’s photonics portfolio. “Someone who has a burn wants to know as soon as possible whether they’re going to need more surgery or not. Plus, the longer you wait to take action, the infection rate goes way up over a few days. The risk of scarring and all the nightmares that go along with scarring go up, too.” According to the current standard of care, it can take up to three days post-burn for laser Doppler imaging, which determines whether the injured tissue is structurally sound enough to be reconstructed. So Durkin’s team developed the cutting-edge spatial frequency domain imaging (SFDI) camera to assess the reconstructive potential of the tissue involved in burns and other wounds.
The SFDI camera uses diffuse optical spectroscopy to take a snapshot of an affected burn area, with the resulting image providing an almost real-time visual map of parameters such as oxygen saturation, water content and total hemoglobin for each pixel. Clinicians can then evaluate tissue viability in wounded areas and determine whether that tissue is a suitable candidate for reconstructive surgery, all within just a few hours. “We think we can buy a couple of days that can dramatically decrease the risk of scars and infection,” Durkin said.
In addition to being a noninvasive technology, the SFDI can differentiate between superficial partial thickness burns and deep partial thickness burns, a relatively muddy area of wound designation within the medical community, according to Durkin. The SFDI, which is being developed and commercialized by California-based Modulated Imaging Inc., recently received a grant to perform a tissue viability analysis in a variety of wounds relevant to the military. As a result, Durkin’s team has received FDA approval for their technology for research purposes and began efforts to secure FDA clearance for a miniature version of the same device at the end of 2017.
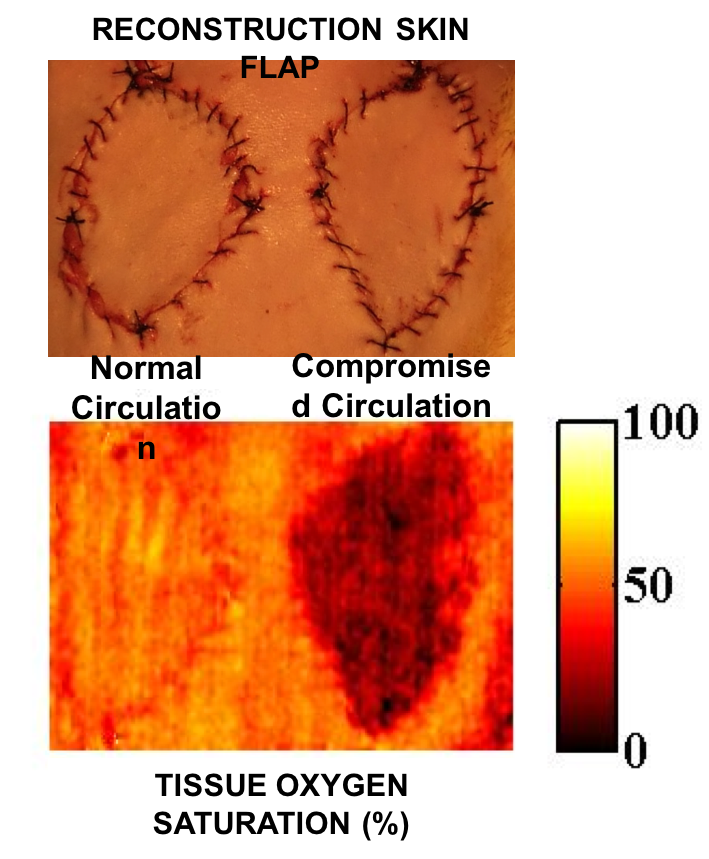
SFDI surgical camera images show reconstruction skin flaps with normal (A) and compromised (B) circulation. SFDI images enable physicians to make early and accurate assessments of tissue viability for burn and wound management, reconstructive surgery and progressive monitoring of grafts and wound healing. (Photo by University of California, Irvine)
CONCLUSION
The fruits of the CCCRP’s military medical mission often translate to the civilian world, and the lactate monitor is no exception. “The diabetes community has caught on to what I’m doing,” Botvinick said, “and they’re very interested in knowing if lactate can help them safely control sugar and exercise routines in diabetes patients.”
For as much effort and investment goes into the CCCRP’s litany of products and projects, so many of those same efforts—tourniquets, a balloon-tipped catheter that stops bleeding known as the REBOA and countless knowledge products—have gone on to improve and save the lives of countless American citizens.
While that is not the stated priority of the CCCRP and its associated technologies, it is a substantial benefit to the taxpaying public. After all, if a resilient military can help develop a resilient population which, in turn, continues to fuel an even more resilient military—well, that’s the very definition of achievement.
For more information, contact Chelsea B. Bauckman at chelsea.b.bauckman.civ@mail.mil or go to http://mrmc.amedd.army.mil/.
RAMIN A. KHALILI serves as the knowledge manager for CCCRP. Before assuming his current role, he spent more than a decade as a broadcast journalist, working in a number of cities across the country. During that time, he earned an Associated Press Award for his work in Phoenix, before securing a position as chief NASA correspondent for CBS in Orlando, Florida. He holds a B.A. in communications from Pennsylvania State University.
This article will be published in the January – March 2018 issue of Army AL&T Magazine.
Subscribe to Army AL&T News, the premier online news source for the Acquisition, Logistics, and Technology (AL&T) Workforce.







